What is the IT Band?
The IT Band stands for the iliotibial band. It is a thick band of fibrous tissue that runs from the outside of your hip to the outside of your knee. It is the accumulation of the fascia from all of the glute muscles and the tensor fascia latae (TFL) (Flatto et al., 2017). Fascia is like plastic wrap around your muscles, or the thin layer of tissue you may have seen around a chicken breast.

The glutes are highlighted in purple, the TFL is highlighted in blue, and the ITB is highlighted in red.
Together, these muscles and the band provide stability to your pelvis and knee in a single leg stance.
What is IT Band Syndrome? What are the symptoms of IT Band Syndrome?
IT Band syndrome is a term used to describe pain or snapping at the lateral hip or knee. It can also sometimes be referred to as “snapping hip” when the snapping occurs at the outside of the hip across the greater trochanter.
Early on, the pain might be intermittent or go away after a warmup. As it progresses in severity, it can become more consistent and the discomfort may increase and affect the entire side of the leg.
The repetitive friction can result in inflammation and irritation of your lateral hip musculature. Other diagnoses that often accompany this lateral irritation include snapping hip syndrome, hip bursitis, and glute medius or minimus tendonitis and tears. (Tatu et al., 2001) At the knee, it can progress into a locking and catching sensation at the lateral knee.
Due to the repetitive high load and the endurance nature of running, IT Band Syndrome can be prevalent in runners (Magalhães et al., 2013). IT Band Syndrome results from imbalances, improper mechanics, or suboptimal loading patterns. Imbalances can be created from not enough variability in workouts or always running or walking on one side of a road or one direction on a track. Pain can occur due to improper shoe wear or insufficient rest between workouts. It can also be due to increasing mileage too quickly, whether running, hiking, walking, or cycling; especially with a lot of downhill work.
Here is a Return to Running Strength Test to assess your loading habits that are needed for running. Make sure to determine not only if you can do these movements, but also what it looks like and what muscles you can feel working.
Sometimes we can get away with movement or habits for a while until they catch up with us, so even if you don’t have pain right now, you can use the assessment as a tool to determine if you’d benefit from these exercises. They can also be part of your injury prevention program to keep you on the road and pain-free.
How do you test for IT Band Syndrome? What are the symptoms of a tight IT band?
Traditionally, an Ober’s test is used by medical professionals to assess for tightness in the IT band. This test is performed in a side-lying position and it evaluates the ability to drop your knee down toward the table (hip adduction range of motion). Limited range indicates a positive test for IT band tightness.
However, a study looking at cadavers showed that the Ober’s test is not a valid way to test IT band length, and that the glute medius, minimus, and hip capsule were more limiting factors for adduction. (Willett et al., 2016) This means it’s essential to look at and address muscle function, pelvic movement, and pelvic positioning rather than just stretching the IT band.
Do you ever have pain in your top hip when you're sleeping? This results from the top leg hanging down and putting low load stress on the lateral hip muscles. This hanging down isn't a problem when those muscles are feeling great, but if they are short or tight, it can be painful. Try putting a pillow between your knees and feet to help relieve some of the pain and reduce the tension being placed on the outside of your hip. As you decrease the stiffness of your glute muscles, pain during sleep will improve and you’ll have less need for the pillow.
What causes IT Band Syndrome?
IT Band Syndrome is due to imbalances in the hips, pelvis, and feet. Studies show that IT band knee pain is connected to foot and arch function, particularly over-pronation and adductor weakness.
How you load through the foot can affect how you load through your hips. However, if you don’t address what’s happening at the hip, then your foot progress won’t stick around long-term.
Adductor strength is associated with the ability to drive the pelvis into internal rotation. This movement helps the body transfer weight over to one leg and springload the glutes for action to push you back to the other side. If you can’t get that movement at the pelvis, it will come from a different plane of motion at the hip or further down at the femur or foot, resulting in poor loading through the lower extremity. This can look like a change in pelvic tilt, femoral internal rotation, or early foot pronation.
Good versus bad internal rotation
Making sure you have dynamic adductor strength will help ensure you don’t compensate elsewhere and improve the loading mechanics through the leg.
When it comes to IT band hip pain, there is an imbalance between the glutes and the tensor fascia latae (TFL).
Healing a painful IT band
Those with IT Band Syndrome often have a more dominant TFL than glutes. This results in collapsing into adduction and internal rotation, both actions that the glutes should control and are driven by the TFL (Flato et al., 2017). This indicates a need for different areas of glute strength, both eccentric and concentric, to control the internal rotation.
How can you fix IT Band Syndrome?
How to stretch or release your IT band
Remember, based on research, instead of thinking, “how can I stretch my IT band?” or “how can I release my IT band?” we should be thinking, “how can I take tension off my IT band?” The tissue is tight for a reason. Stretching it doesn’t change why it's tight or help you gain dynamic strength. You must instead address pelvic positioning and muscle function.
Should I foam roll my IT band?
Foam rolling your IT band doesn’t influence its length. However, foam rolling the muscles, glutes, and TFL can significantly decrease the tension put on the IT band. (Hall & Smith, 2018). That being said, the results only lasted for 10 minutes (D’Amico et al., 2021). You can use foam rolling to help down-regulate tissue, but once again, it comes back to addressing pelvic positioning and muscle function to elicit more permanent changes.
What are IT band exercises?
Addressing pelvic positioning
Remember how the Ober’s test indicates it is muscle tension that affects the range more than the IT band length itself? The research took it a step further and proved that addressing the position of the pelvis through activation of the hamstrings and lower abs reduced an anterior pelvic tilt and improved inlet internal rotation. Decreasing tension in the lateral hip musculature improved the Ober’s test results and immediately reduced pain (Tenney et al., 2013). Addressing pelvic positioning through muscle activation can change the length-tension relationship of other muscles, affecting how they function.
Changing alignment affects which muscles are set up to do the work. A pelvis that lives in a more tipped-forward posture (anterior pelvic tilt) positions the TFL at a greater advantage to work, and the glutes in a less efficient position to function. This also changes the alignment of the other hip muscle fibers, such as the glute med and piriformis.
A tipped-forward pelvis increases piriformis activity and positions it to do the job of the glute med in stabilizing the pelvis. The glute med is then weakened, setting it up for decreased function and a potential muscle strain. A more active piriformis can also contribute to the femur being shoved forward in the socket, further inhibiting glute max function and worsening hip imbalances.
Activation of the proximal hamstrings can reorient the pelvis, inhibit the TFL, and set up the rest of the hip muscles for better function. The trick is finding them in isolation so the relative movement can dynamically occur in the pelvis, allowing for full glute function.
Here are some exercise variations to work on this:
Getting hamstrings without glutes to unstick the sacrum
Hamstring bridges
Strengthening the hips
Once you have improved the positioning of your pelvis, then it’s all about loading and strengthening your hips in this new position.
The hip can move in three planes of motion; frontal, sagittal, and transverse.
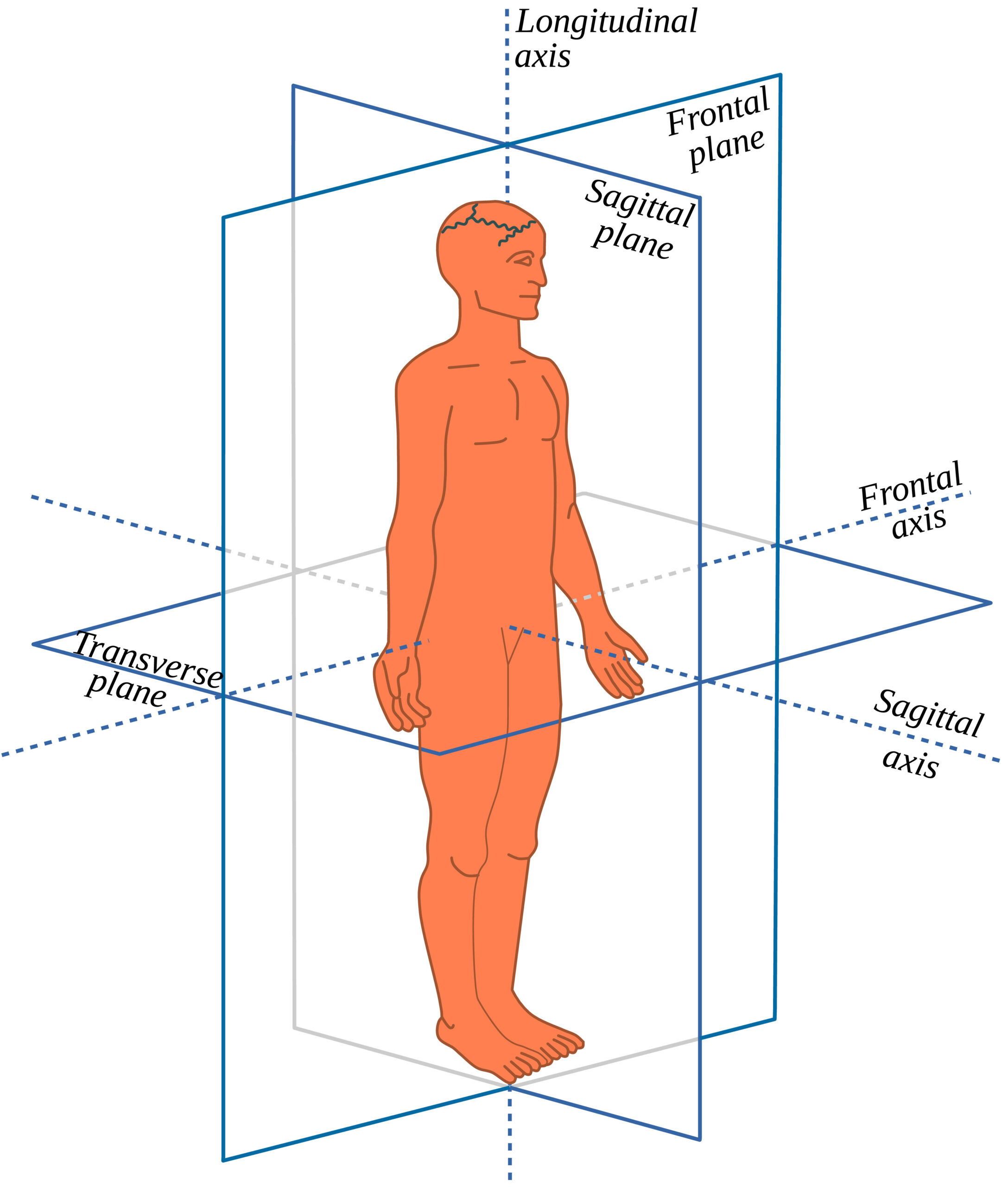
If you don’t have dynamic strength and stability in all of them, you will overuse one plane of motion. This is often accompanied by a change in orientation of the pelvis (falling into an anterior or posterior tilt, hiking a hip, or rotating one side) instead of the relative movement we want to occur at the pelvis and in the muscles.
Think of muscles as a rubber band that you want to stretch to load so they can then contract well. You must lengthen under load first to set it up for a good contraction. To optimize hip function, you need to ensure you don’t work only at one end range, but strengthen through a full range to gain control in all directions.
Why glutes need internal rotation work:
Also, remember that not all glute strengthening is equally helpful. By knowing your goal – whether to shorten or lengthen, strengthen or inhibit – you can pick which direction you need to work on first and progress your glute exercises accordingly.
Glute Max
Bringing your glute max into the sagittal plane can help you work on full-range hip extension, further inhibit your TFL, and set up a better position to work on eccentric glute lengthening.
Looking at what happens in a single-leg bridge can help you assess your stability and pelvic positioning in a single-limb stance.
Single leg bridge without hip flexors or back:
Are you able to keep your TFL soft and squishy? Can you avoid falling into an anterior pelvic tilt or letting your pelvis tip to the side? Can you still use your hamstrings and glutes rather than your back and quads?
You can also pay attention to what is happening with your feet, as that can affect what’s happening at your knee or hip. Can you maintain equal contact between the base of your big toe, pinky toe, and heel throughout the movement? Does your knee like to collapse in or turn out?
Here’s a variation to help ensure the glute max shows up for your hip extension without compensating at your foot.
Bridge with a tibial twist for knee pain:
Sometimes starting with a foot-elevated bridge can help make it easier to access your hamstrings to work on improving pelvic positioning first, or to make sure your quads aren’t doing all of the work. Then you can progress the movement to a hip thrust, taking the glutes through a larger range of motion and working more glute max over hamstrings.
Bridges versus hip thrusts:
For either version, you may need more adductor work to improve pelvic positioning in the frontal plane and help down-regulate the deep hip rotators and isolate more glute max.
Add an adductor squeeze to glute work for piriformis relief:
It’s all about finding the right variation that brings better balance to your system. The variation that feels better can also give you greater insight into what your body needs more.
As an aside, if you’re having a hard time getting the TFL to calm down, it responds well to some neuromuscular dampening by foam rolling, so give that a shot before trying the exercises.
You'll need glute med and adductor strength to transition to more dynamic, single-leg glute max strength.
Glute Med
Research shows that those with a greater degree of hip pathology had more significant atrophy (or muscle wasting) of the glute medius (Perry et al., 1983), and runners with IT band pain had noted glute medius weakness (Connelly et al., 2020; Allison et al., 2016).
In one research study, a group of runners was put on a glute med strengthening protocol for six weeks. At the end of the six weeks, 90% were pain-free with running, and were still running pain-free at the end of 6 months. (Fredericson et al., 2000). The important thing to note about this group was not only did they work on increasing glute med strength, but endurance as well (3x30 reps). They also eliminated any activity that caused pain for those six weeks, allowing the aggravated tissue to have some rest.
Let’s break down the glute medius even further. It is divided into three different portions, each with a different action. The posterior portion does external rotation, helping to stabilize the femur in the socket. The medial portion does abduction, to help prevent hip drop in a single limb stance. The anterior portion does internal rotation, helping to rotate the pelvis in gait and keep the femur centered in the socket. It has also been shown to be an anticipatory muscle in preparation for heel strike (cite Retchford et al. from PP anatomy section).
Working together equally creates balance in the dynamic function of the glute medius, joint centration at the hip and pelvis, and knee stability. This also helps to create harmony between the adductors and deep hip rotators so nobody gets overworked.
As I mentioned, not all glute exercises are created equally, so making the appropriate exercise selection and order of operations are both important. This allows you to strengthen a weakened muscle with the right support team instead of going for the kill and trying to cheat your way into making a movement happen.
Research shows significant variability in which muscles are used in traditional glute medius strengthening exercises, such as clamshells and side-lying or standing leg lifts. (cite Moore et al., 2020). Some of this variability is due to exercise execution. It’s not just what you do, but how you do it. The timeline for adding in an exercise is also important. A muscle may be weak, but it may need a better foundation or support system before it’s asked to work. Finally, these commonly used exercises often only focus on end-range concentric engagement. Functional strength is being able to take a muscle through its full range with control.
Check out this article for more information on when clamshells are right for you, as well as another clamshell variation that can help target more glute max. More glute max is often needed to help balance an overworked glute medius.
Studies also show that these traditional glute medius strengthening exercises did not target the often weak anterior glute medius, making the point again that not all glute exercises are the same. A well-functioning anterior glute medius helps bring balance to the deep hip rotators and TFL, resulting in an overall joint centration effect of the femur and a stable pelvis.
The anterior glute medius can be isolated by performing hip hikes and femoral internal rotation. The trick with both is ensuring that your glute medius is doing the work. Make sure you address your pelvic positioning first with the proximal hamstring. Maintaining a neutral position throughout the movement will help keep the TFL and deep hip rotators out of it.
You can also work on femoral internal rotation in a more traditional reverse clam position. As you do it, maintain active core engagement and a steady pelvic position throughout the movement. You can use a block between your knees to isolate the femur moving in the socket. You can also perform the same movement in a hands and knees position to add more core stability. Feel free to add a band to both versions as tolerated.
Let’s look at progressing into hip hikes, as they can be great to translate into function. Remember that it can be very challenging to feel these in the right place.
If you tend to have overactive deep hip rotators, performing hip hikes in a hinged position can help keep them lengthened as you drive the movement from the glute med and work on the frontal plane control that is needed for a weight transfer through the pelvis.
Standing hip shifts
When transitioning to upright, an isometric hold can be a great way to work on the transition from double leg to single leg. It can also serve as the starting point for dynamically controlling a muscle through its full range, allowing for both mobility and strength.
You can progress this exercise into doing a wall squat while maintaining the press out. Then, you can eventually progress toward a single-leg squat for the ultimate test of single-leg hip strength and control. Always make sure you don’t lose any of the previous components of good form and that you feel it in the right place as you advance the exercise.
Finally, the full upright hip hike will help isolate more of the anterior glute med.
Hip hikes
It’s important to ensure that your glute medius is doing the work instead of just your adductors. Otherwise, that can cause a collapsing in of the knee, contributing to IT band pain.
Suppose you are unable to find your glute medius due to difficulty with stabilizing your pelvis and foot. A different variation of isolated glute medius strengthening might be needed at first.
This can bring you back to the side-lying leg lifts. They can be a great way of “waking up” the glute med and they provide the pelvis with more stability because you’re lying on the ground. However, as previously mentioned, it’s not just about what you’re doing, but how you’re doing it. Check out this clip on refining side-lying adductor glute lifts to ensure you get the most bang for your buck.
Just because a muscle is bulky doesn’t mean it is strong or can work dynamically. With all glute medius work, you want to ensure that you can not only concentrically contract it but also eccentrically lengthen it under control. This means paying attention to how you eccentrically load during the above exercises and making sure the femur isn’t being shoved forward in the socket with overactive deep hip rotators showing up more than the glute max.
Depending on your specific needs, you can also vary how you hold a weight in any split stance or single-leg exercise. Finding better control in the frontal plane during a sagittal plane exercise will help your glute max get stronger.
Holding weight for single-leg activities
If you’re progressing toward single-leg exercises, start with holding the weight on the same side as your front leg. This will give a little assistance to your glute medius. Think of it as an isometric hold in one plane of motion while dynamically working in another. Isolated glute medius work will help it get stronger to “hold you in from the sides” so you can sit straight back into your hips and lengthen your glute max. As the glute medius gets stronger, you will progress to switching the hold to the opposite hand to increase the challenge and load on the glute medius.
On the flip side, if you have more distal IT band pain at the knee, you might need to progressively overload by challenging the adductors more in these patterns, which means doing the opposite.
Adductor strength
If you noticed that you have a tendency toward overactive deep hip rotators, IT band knee pain, or you benefited from the bridge while squeezing a block, then adductor work could help bring better balance to your system.
Isometrically, adductors can help put the pelvis into a position that inhibits the deep hip rotators to isolate more glute max. The adductors will also drive internal rotation at the pelvis, which can help with eccentric lengthening of the glute max, deep hip rotators, and glute med. This loads the leg more effectively and positions the muscles in a better place to shorten and push off from.
Why glutes need internal rotation
With closed chain internal rotation work, we want the motion to come from the pelvis and not the femur. This will ensure that the glutes are getting eccentrically lengthened instead of allowing the knee to collapse and contribute to IT band pain.
Then, just like any other muscle, you want the adductors to be able to dynamically lengthen and shorten. Adductor slides can be a great way of working on weight shifts to progress toward single-leg activities.
Adductor slides
When working the adductors, make sure the TFL is relaxed to help maintain good pelvic positioning and subsequent glute function.
Core strength
Core control is another area to address to help set up your hips for more success. Your hip muscles can be the big movers and drivers of pelvic positioning, but core strength will be the glue that holds it together. Core strength for pelvic stability includes feeling supported by your lower abs, particularly in a single leg stance.
Check out this video for a series on progressing through lower ab stabilizing leg lift exercises:
Abdominal progression
Then you can use side planks to assess more single-sided strength. They can also provide another opportunity to bias your hip strengthening, depending on what you need more of. You can get more glute medius if you stack one leg on top of the other, or more adductor if you do a Copenhagen side plank.
If you’re having a hard time with an overactive TFL and finding your lower abs or have a weak lower glute med, then using the hamstrings can set your plank up for more success.
Finding hamstring in side plank
Then, taking that strength into a dynamic rotation can help with the cross-connection between the upper and lower body that is needed for running.
Connecting with the feet
Lastly, if you found that the bridge with the sock under your arch felt the best or you tend to have pain at the outside of your knee, addressing what’s happening at the foot will be an important part of your recovery.
There's a little test to see if your hip tightness is affecting your arches, and vice versa:
Hip tightness affecting arches
Limitations in tibial internal rotation or a bias into external rotation can often be due to compensation at the tibia in response to the femur collapsing in. The ability to internally rotate your tibia can affect how you bear weight through your foot and the mechanics at the knee. If you’re lacking range of motion here, you’ll be creating extra tension across the knee and foot, making both unable to load well.
Tibial internal rotation mobilization video
Looking at your mid foot function addresses how you distribute load through the entire kinetic chain and can help with eliminating overpronation. Just because you have a high or low arch doesn’t mean that it functions well. Like any other area of the body, we need to make sure it can move through its full range with good control and without compensating elsewhere. This not only entails looking at the mid foot and arch, but also at the ankle and calf.
Here is a series on foot and calf mechanics to dive deeper into that topic:
Yoga toes and waking up your big toe
To take your dynamic foot function to the rest of the kinetic chain, you can apply wedges or foot props to help set up how you load your foot and also your hips.
Wedges for a lunge video
Drive IR from the ground up
As your feet and hips become dynamically more mobile and stronger, you won’t need the wedges; but they can be a great prop to help assist your body to move in a more balanced way.
What exercises to avoid with IT Band Syndrome?
To keep it simple, don’t do exercises that aggravate your symptoms. Watch the alignment of your pelvis and knees, and pay attention to what you’re feeling during the exercises. Make sure to pick the right variation where you can successfully perform the exercises without just going through the motions. With running, correcting form in the moment can be challenging without compensating elsewhere. Think of the exercises mentioned above as giving you the tools to help it happen naturally.
When can I return to activity?
The work you do during this time to develop more balanced strength may also act as injury prevention in the future. This might mean taking a break for now from your preferred activity, such as running. I know this can be mentally and emotionally painful! However, think of it like this; if you’re always punching a bruise, it’s going to be hard for that bruise to heal even with all the good things you may be doing for it. It might feel like forever, but it will only be a minor blip in the big picture.
In the end, it’s not about foam rolling or trying to stretch the IT band, but more about addressing the muscles that affect it and the movement patterns that can contribute to putting it in a position of chronic tension.
The amount of time this takes varies per individual, depending on their base level of strength, neuromuscular connections, and what they’re looking to get back into doing. It can take 4 or 6 weeks of consistent training, progressive overload with proper form and muscle activation, and taking a break from aggravating activities to note some improvements. The more mileage or varied terrain you’re looking at, the more strength and endurance you’ll need for your activity.
Remember, your body will communicate with you what it’s feeling and what it needs. It will start as a whisper, but if you keep ignoring it, it will turn up the volume and become a scream. So even if you’re not having pain that is very bad right now, it might still be a good time to pause and reflect on what your body is telling you. Assessing your movements and implementing a balanced strength training program before symptoms get worse can help you keep doing what you love with fewer bumps along the way.
References:
- Tatu L, Parratte B, Vuillier F, Diop M, Monnier G. Descriptive anatomy of the femoral portion of the iliopsoas muscle. Anatomical basis of anterior snapping of the hip. Surg Radiol Anat. 2001;23(6):371-374.
- Magalhães E, Silva AP, Sacramento SN, Martin RL, Fukuda TY. Isometric strength ratios of the hip musculature in females with patellofemoral pain: a comparison to pain-free controls. J Strength Cond Res. 2013;27(8):2165-2170.
- Willett GM, Keim SA, Shostrom VK, Lomneth CS. An Anatomic Investigation of the Ober Test. Am J Sports Med. 2016;44(3):696-701.
- Flato R, Passanante GJ, Skalski MR, Patel DB, White EA, Matcuk GR Jr. The iliotibial tract: imaging, anatomy, injuries, and other pathology. Skeletal Radiol. 2017;46(5):605-622.
- Hall M, Chadwick Smith J. THE EFFECTS OF AN ACUTE BOUT OF FOAM ROLLING ON HIP RANGE OF MOTION ON DIFFERENT TISSUES. Int J Sports Phys Ther. 2018;13(4):652-660.
- D’Amico A, Silva K, Gallo J. Time Course of Acute Hip Adduction Range of Motion Changes Following Foam Rolling. IJSPT. 2021;16(2):431-437.
- Tenney HR, Boyle KL, Debord A. Influence of Hamstring and Abdominal Muscle Activation on a Positive Ober's Test in People with Lumbopelvic Pain. Physiother Can. 2013;65(1):4-11.
- Lyons K, Perry J, Gronley JK, Barnes L, Antonelli D. Timing and relative intensity of hip extensor and abductor muscle action during level and stair ambulation. An EMG study. Phys Ther. 1983;63:1597-1605.
- Connelly CM, Moran MF, Grimes JK. COMPARATIVE ANALYSIS OF HIP MUSCLE ACTIVATION DURING CLOSED-CHAIN REHABILITATION EXERCISES IN RUNNERS. Int J Sports Phys Ther. 2020;15(2):229-237.
- Allison K, Wrigley TV, Vicenzino B, Bennell KL, Grimaldi A, Hodges PW. Kinematics and kinetics during walking in individuals with gluteal tendinopathy. Clin Biomech (Bristol, Avon). 2016;32:56-63.
- Fredericson M, Cookingham CL, Chaudhari AM, Dowdell BC, Oestreicher N, Sahrmann SA. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med. 2000;10(3):169-175.
- Retchford TH, Crossley KM, Grimaldi A, Kemp JL, Cowan SM. Can local muscles augment stability in the hip? A narrative literature review. J Musculoskelet Neuronal Interact. 2013;13(1):1-12.
- Moore D, Semciw AI, Pizzari T. A SYSTEMATIC REVIEW AND META-ANALYSIS OF COMMON THERAPEUTIC EXERCISES THAT GENERATE HIGHEST MUSCLE ACTIVITY IN THE GLUTEUS MEDIUS AND GLUTEUS MINIMUS SEGMENTS. Int J Sports Phys Ther. 2020;15(6):856-881.

